CONCORD, N.C. — Four months after North Carolina overhauled the state's Medicaid program, some small businesses continue to wait for tens of thousands of dollars in unpaid claims.
"I'm very disappointed as an owner," Royal Orthotics Owner Corey Peña said. "I can't be the only one going through this.'"
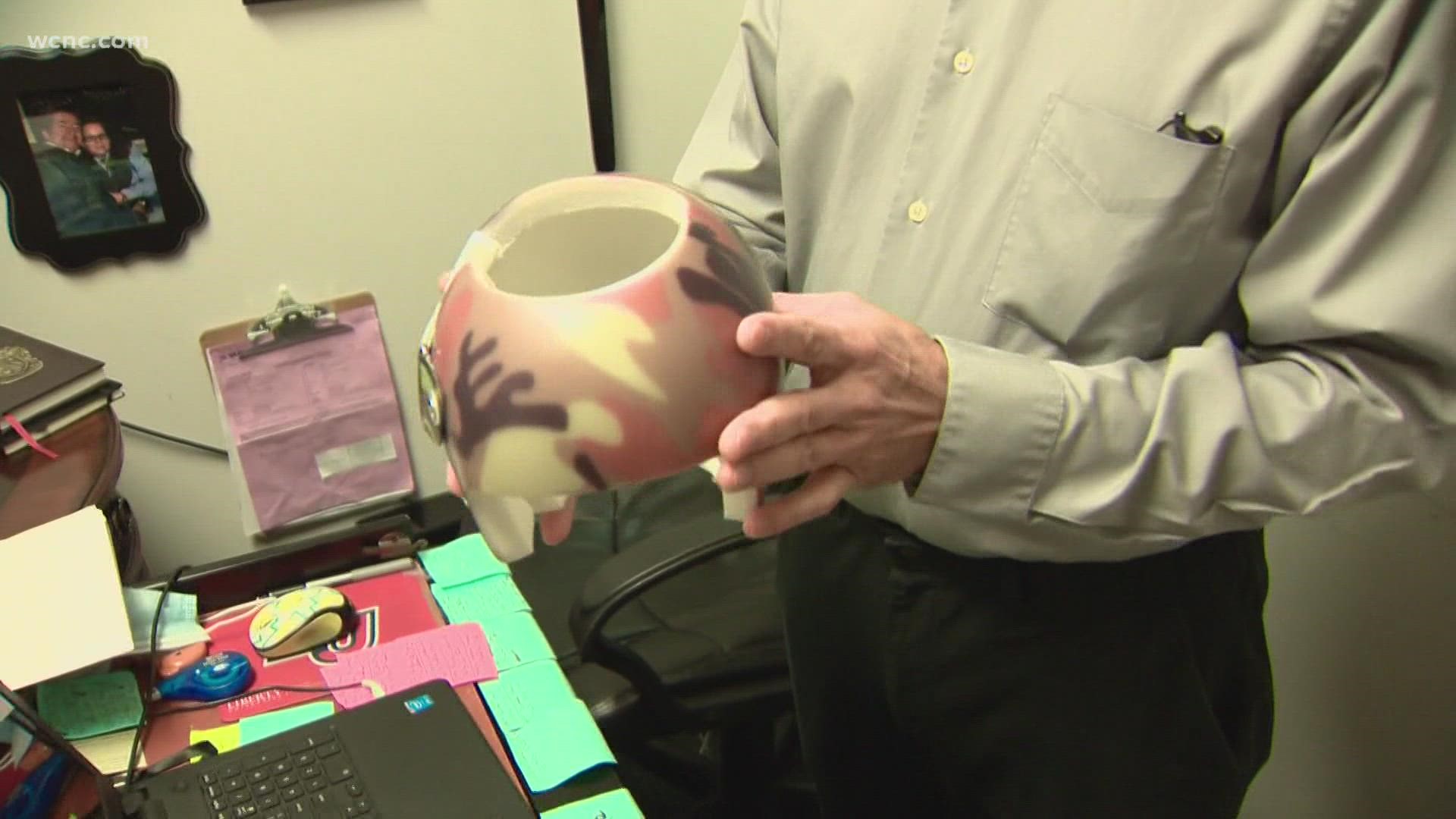
Peña, who specializes in helping kids with cerebral palsy and spina bifida, said most of the children he treats are on Medicaid. However, since the state transitioned to NC Medicaid Managed Care on July 1, he said three of the five companies now handling claims are not fully reimbursing him for services. He said the companies own him more than $45,000 combined.
"I love what I do. I love taking care of these children, but it's starting to tie my hands," Peña said. "We're in November and virtually almost nothing has changed for us."
Long before North Carolina handed over control of its Medicaid program to private companies, Peña said he prepared for bumps in the road, but four months in, he said he never expected to be taking a hard look at the future of his business.
"I don't like thinking about it," Peña said. "I don't want to go there, but as an owner, I have to make serious considerations of the possibilities."
State data show he's not the only provider who has raised questions. Records show the Medicaid Provider Ombudsman has opened more than 400 cases a month since July.
"Many of the calls to the Provider Ombudsman are to address questions, rather than complaints," North Carolina Department of Health and Human Services Press Assistant Catie Armstrong said. "From July through Oct., the provider ombudsman received 2,255 calls and emails, of which 1,985 have already been resolved. NC Medicaid has more than 96,000 providers and over 10 million managed care claims have been processed since July 1, 2021."
Overall, the agency has considered the transition, years in the making, a success, but in Aug., amid questions from providers and WCNC Charlotte, North Carolina Medicaid Deputy Secretary Dave Richard acknowledged room for improvement.
"It's not acceptable," Richard said of delayed payments at the time. "We're fixing it, if I was the organization that wasn't getting paid, I would feel exactly as they do."
In the three months since, speech therapists who previously waited to get paid now say their payments are consistent, but all is not equal. Two mental health providers in different parts of the state told WCNC Charlotte they're still waiting to get reimbursed; one is out more than $50,000 in unpaid claims.
"Medicaid remains committed to ensuring that providers continue to get paid for delivering care and services to Medicaid beneficiaries after we launched NC Medicaid Managed Care on July 1," Armstrong said. "While in managed care providers are paid by the health plans with which they often have contracts, this is a new process for all involved. Therefore, through a combination of proactive outreach to providers, daily meetings with the health plans and addressing issues received through the new NC Medicaid Help Center, NC Medicaid is well-positioned to hear and respond to provider concerns. We understand that while most providers are getting paid, some providers are having issues and we continue to support them through this transition. Providers are encouraged to work with the health plans to resolve their issues and may request a 'hardship payment' while those issues are being worked out. If providers do not get the resolution they expect, they may contact the Medicaid Provider Ombudsman who will work with the health plan and provider to escalate the claims problems and provide technical assistance if necessary."
Peña said he has reported his problems to the Medicaid Provider Ombudsman. The Concord small business owner said he and his staff have also met with managed care representatives to fully understand the changes.
"(They say), 'Just hang on. Just hang on another month,'" Peña said. "It's been since the beginning of July."
WCNC Charlotte shared Peña's information with the North Carolina Association of Health Plans, hoping the organization can help him collect his payments.
The state's Medicaid program serves 1.6 million low-income adults, kids, pregnant women, seniors, and people with disabilities across North Carolina.
WCNC Charlotte is always asking "where's the money?" If you need help, reach out to the Defenders team by emailing money@wcnc.com.
Contact Nate Morabito at nmorabito@wcnc.com and follow him on Facebook, Twitter and Instagram.