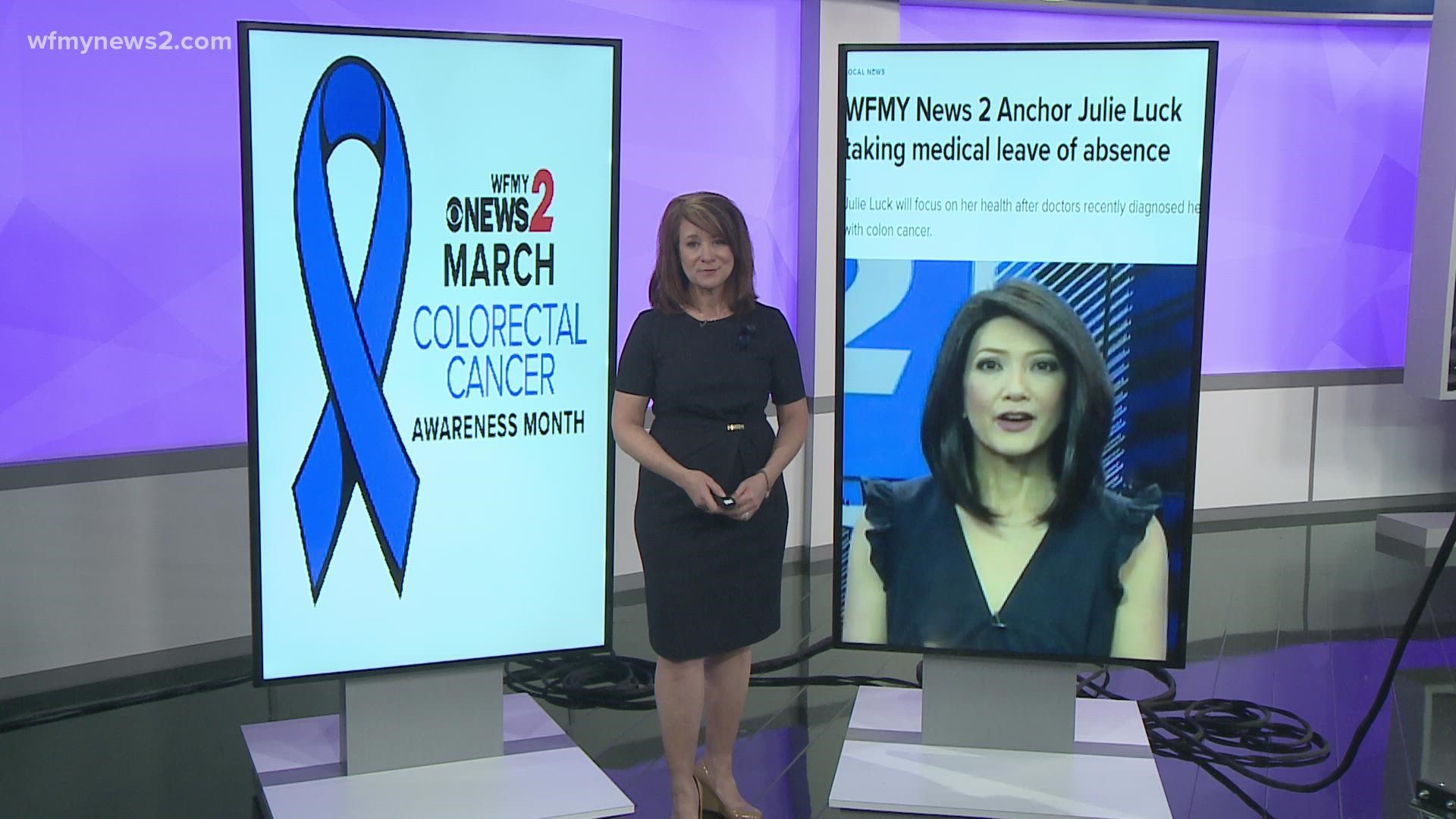
GREENSBORO, N.C. — This day and this month of Colorectal Cancer Awareness is personal to us here at WFMY News 2. Our own Julie Luck was recently diagnosed after a routine colonoscopy.
Today, as we raise awareness, the News 2 family is wearing blue in some form or fashion. Many have posted themselves wearing blue or a blue ribbon. Some faces and names you'll recognize, some you won't, but all of them are on #TeamJulie. All of us are looking forward to the day she is cancer-free.
Over and over again, Julie has used her voice to urge people to get screened. In May of 2021, The US Preventive Services Task Force revamped their recommendation to include screenings for those 45 to 75 years old. Previously, it was 50 to 75 years old. To be clear, the screenings can include at-home tests as well as colonoscopies - it's not colonoscopies alone.
2 Wants To Know and Consumer Reports looked into some of the at-home screening tests.
Cologuard is an at-home test to screen for colon cancer. Some folks who have used this at-home test are getting surprise medical bills. Under the Affordable Care Act, only routine screening tests are covered.
If you take this at-home test and the result is positive, then oftentimes your follow-up colonoscopy can be coded as an uncovered "diagnostic" test. The colonoscopy would have been fully covered if the Cologuard test hadn't been used first.
Cologuard now has a new language on its website saying although "millions of patients have access to this follow-up colonoscopy with no out-of-pocket costs...not all do".
As always, talk to your doctor and look at what's covered to find the best screening tool for you.