Faced with skyrocketing costs for insulin to treat his type 1 diabetes and limited insurance options, earlier this month James Jay Fortin, of York, Maine, had to get creative. He and his partner turned to the online fundraising platform GoFundMe to ask friends and strangers for donations.
In less than 48 hours, they had exceeded their modest goal of $1,300, ultimately raising $8,910. “Jay needs insulin to survive, plain and simple,” says Joanne Muckenhoupt, Fortin’s partner, who sponsored his GoFundMe campaign. “Yet, as costs go up, and our income stays the same, what can we do?”
According to the American Diabetes Association, more than 7 million people in the U.S. depend on insulin, which regulates blood sugar. But the cost of this life-saving drug has shot up in the last five years.
Some commonly prescribed types have experienced the biggest price hikes since 2014, including Novalin (up 51 percent), Humalog (up 63 percent), and Novolog (up 72 percent), according to figures from GoodRx, which tracks drug prices, provided exclusively to Consumer Reports. Another common type of insulin, Alfrezza, has skyrocketed 90 percent since 2015.
Because of rising costs, 1 in 4 people who rely on insulin say they cut back on the amount they use to save money, according to a 2018 survey in the Journal of the American Medical Association. Rationing insulin can have “very serious and sometimes deadly consequences,” says LaShawn McIver, senior vice president of government affairs and advocacy at the American Diabetic Association.
There are several reasons why consumers are facing such high insulin costs, including drug companies charging more for newly developed forms of the drug and a lack of low-cost generic options.
While solutions to those and other underlying problems could still be a way off, pressure to ease the insulin affordability crisis is growing—and beginning to have results. New programs from pharmaceutical companies and insurers, and some new federal and state government rules, are being put in place to help the many people like James Jay Fortin right now.
How Did Insulin Get So Expensive?
Insulin price increases of the last few years caught the attention of Congress, which in 2018 and 2019 held multiple hearings with CEOs of the three companies that make insulin in the U.S.—Eli Lilly, Novo Nordisk, and Sanofi. They wanted an explanation.
One reason the manufacturers gave is innovation. Regular insulin—which has been available for nearly 100 years—has long been so cheap that no company bothered to make a generic version of it. But it was also inconvenient, requiring people to give themselves multiple shots a day. So drug manufacturers developed new types of insulin: long-acting, medium-acting, and rapid-acting, as well as various hybrids, which only had to be used once or twice a day and offered more consistent glucose control.
Companies say these new versions give people with diabetes better options. But by developing them, they were also able to create expensive, branded products.
And because many people with diabetes need the drugs to survive, companies could charge almost whatever price they wanted—and increase those prices repeatedly, says Vincent Rajkumar, M.D., from the Mayo Clinic in Rochester, Minn., who has studied and written on this topic. “We have a vulnerable population of millions willing to pay anything to have access to lifesaving drugs,” he says.
There’s another force at work that causes the price of insulin and other drugs to rise—the complex drug rebate system.
A rebate is money a drug manufacturer pays middlemen in the insurance industry—called pharmacy benefit managers, or PBMs—to get their drugs covered by insurance companies. As those rebate payments have increased, so has the cost of insulin, according to research by Adam Fein, an industry consultant and drug pricing expert at the Drug Channels Institute, a research firm.
For example, between 2014 and 2018, Fein notes that Eli Lilly’s insulin drug Humalog went up by 52 percent, from $391 per patient, per month to $594. During the same time period, the amount Eli Lilly paid PBMs and other middlemen in rebates jumped 88 percent, from $244 per patient, per month to $459.
Getting Costs Under Control
The Trump administration and Congress have recently proposed some ways to rein in insulin prices.
For example, the Trump administration, Health and Human Services, and the Food and Drug Administration have proposed letting retail pharmacies, drug wholesalers, states, and even drug manufacturers purchase expensive drugs, including insulin, from Canada, at cheaper prices. The FDA has also crafted a plan to develop a quicker pathway to approve less-expensive generic versions of the newer insulin drugs.
And bills introduced last year in both the House (H.R. 4906) and Senate (S. 2199) would incentivize drug companies to roll back insulin prices to 2006 levels and prohibit insurance companies from forcing patients who need insulin to first meet a deductible before their insurance kicks in.
While passage of those measures could still be a long way off, the big three insulin manufacturers have recently rolled out programs that could provide relief to consumers more quickly. Additionally, some insurance companies and PBMs have started to offer programs to help contain what consumers must pay.
Here’s how you can take advantage of these new options, as well as some older ones, to lower insulin costs.
Check Your Out-of-Pocket Limit
Federal guidelines issued last year made it possible for health plans to cover insulin costs before consumers meet their deductibles, in the same way a doctor’s visit for an annual checkup is covered, says Brian Marcotte, CEO of Business Group on Health, an organization that represents large employers to address the healthcare needs of their employees. That change prompted some PBMs and insurance companies to offer other programs that limit consumer copays and other out-of-pocket expenses for insulin, Marcotte says.
For example, the PBM Express Scripts now offers plans through Cigna insurance that have copays of $25 or less for a 30-day supply of insulin, says company spokesperson Jennifer Luddy. Plans representing more than 6 million people across the country have enrolled so far, she says.
Oscar Health in New York announced this month that some of its plans would limit insulin copays to just $3.
CVS Health, another PBM, will offer a plan with zero-dollar copays for insulin starting in 2021, says Trey Hollern, spokesperson for CVS Health. He notes the company already offers that to its own 300,000 employees.
Marcotte expects more insurers and employers will offer these plans in 2021. But, he says, “check your health plan now to see if they’re already available.”
Some states are also limiting the out-of-pocket for insulin that an insurer can charge. Colorado and Illinois have already passed laws that require employers to limit an employee’s out-of-pocket insulin costs to no more than $100 per month. Florida, Massachusetts, Michigan, New Jersey, New York, Pennsylvania, and Wisconsin have introduced, but not yet passed, similar legislation.
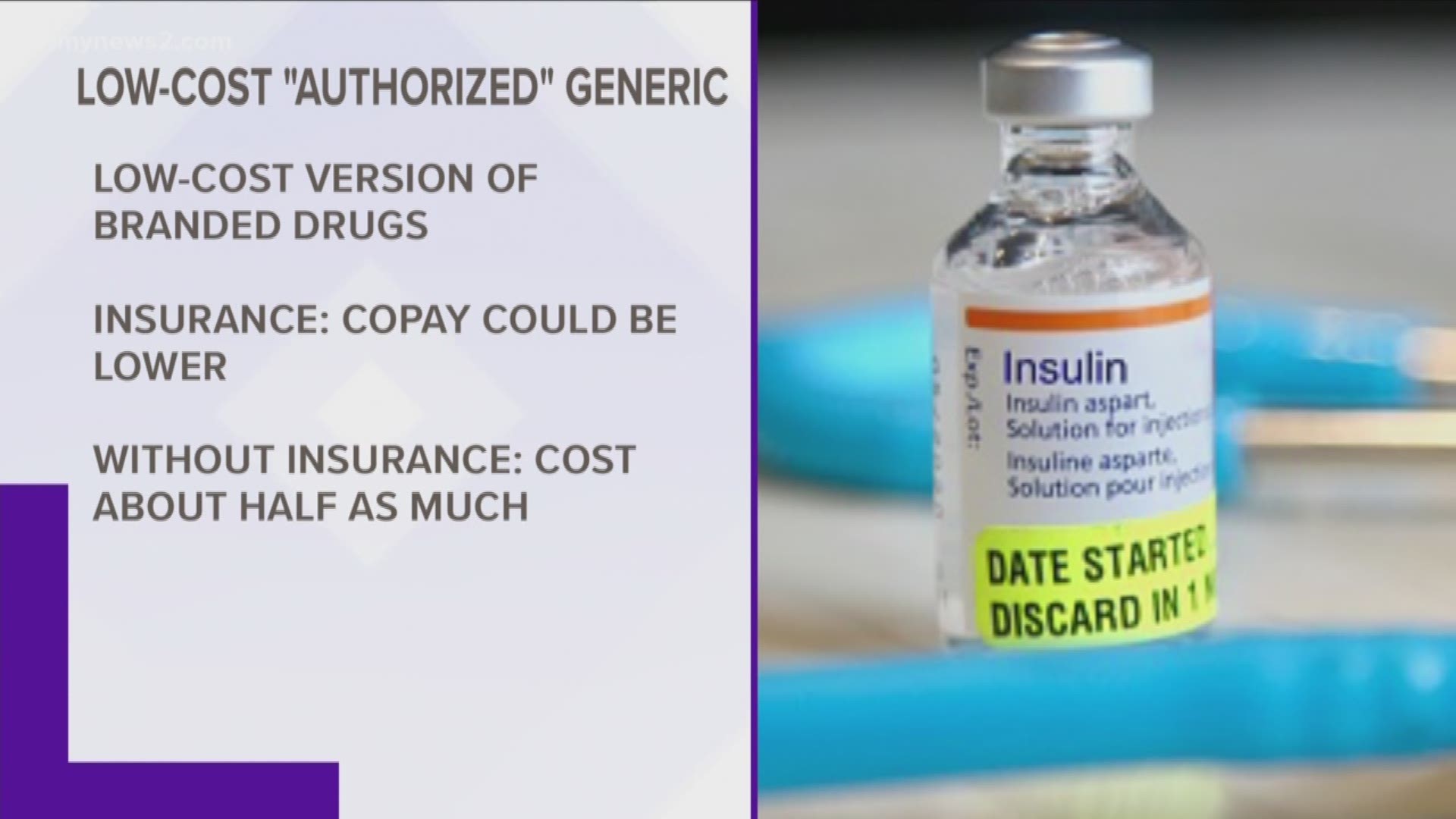
Consider a Low-Cost ‘Authorized’ Generic
These can be especially good options if your insurance plan has not yet set low or zero copays for insulin, or if you don’t have insurance.
“Authorized” generics—which insulin drug manufacturers began introducing last year—are essentially low-cost versions of a company’s branded drug. And because they are chemically identical, pharmacists in most states can fill your prescription with one even if your doctor prescribed the branded version.
For someone with insurance, a copay could be lower with these authorized generics than the are with branded versions. And if you don’t have insurance, or can’t use it for some reason, they typically cost only about half as much.
For example, Eli Lilly’s authorized generic version of Humalog, called Insulin Lispro, is half the cost of the branded version, says company spokesman Greg Kueterman. Without insurance, that would cost a consumer about $150 for a 30-day supply. The company will have discounted generic versions of Humalog 75/25 and Humalog Junior Kwikpen in April, Kueterman says.
In January, Novo Nordisk began offering generic versions of two of its popular insulins, Novolog and Novolog Mix, at a 50 percent discount.
If your pharmacy doesn’t carry the low-cost insulin you’re looking for, ask a pharmacist to order it, says Vic Curtis, vice president of pharmacy at Costco. Expect delivery to take one to two business days.
Sanofi doesn’t have an authorized generic insulin, but does have other low-cost options for its branded drugs (see below).
Look for Inexpensive Branded Drugs
There are some lower-cost options now available for people who want to or have to stick with a branded insulin.
Sanofi, for example, now has a program for people who buy their own insurance or get it through their employer that eliminates or sharply reduces copays for five of its branded drugs: Adlyxin, Apidra, Lantus, Soliqua 100/33, and Toujeo. For people without insurance, it sets a $99 limit per month for four of its drugs: Admelog, Apidra, Lantus, and Toujeo, says Nicholas Kressmann, spokesperson for Sanofi.
Eli Lilly has set a similar cap—$95 per month—for Humalog, Humalog Mix 75/25, KwikPen, and Humalog Junior KwikPen. The discounted price should be automatically available when you fill your prescription, says Eli Lilly spokesperson Kueterman. People without insurance can use a discount card to get the same low price (call 833-808-1234 Monday-Friday, 9 a.m. to 8 p.m ET), says Kueterman.
Last month, Novo Nordisk announced it would offer a month’s supply of any of its branded insulins, including Levemir, Novolin, Novolog, Novolog Mix 70/30, Ryzodeg, and Tresiba for $99 for anyone with or without insurance, says Ken Inchausti, spokesperson for Novo Nordisk.
See If You Qualify for Free Insulin
Drug companies offer free insulin to people below certain income thresholds, says Rich Sagall, M.D., president of Needymeds, a nonprofit organization that helps consumers find discounts and savings programs on thousands of medications.
The problem of finding affordable insulin is so widespread that it’s the second-most common reason patients contact his group, Sagall says. (The blood thinner Eliquis is the top reason.)
In mid-2019, these programs—called patient assistance programs—raised that cutoff to 400 percent of the federal poverty level, which is $50,000 for a single person or $103,000 for a family of four, Sagall says. That means more people may be able to qualify.
Still, there are some caveats. One is that these programs can be discontinued or change their income or other qualifications at any time.
Plus, Sagall says, don’t expect to receive the medications right away. It often takes up to two weeks from the time you fill out the forms till you receive the insulin. While some companies have made it easier to submit applications, it will still take several working days before a decision is made.
Another caveat is that these programs apply only to people who don’t have insurance or those whose insurance doesn’t cover a company’s drug. And you likely won’t qualify if you have Medicare, Medicaid, or insurance from a federal source such as the Veteran’s Administration, Sagall says. Though do check back periodically, he says, because the qualification requirements can change.
For more about these programs from the three insulin makers:
Eli Lilly’s LillyCares (800-545-6962). In emergencies, you may be able to get a free, limited supply by calling customer service at 833-808-1234.
Novo Nordisk’s NovoCare program (844-668-6463). In emergencies, you may be able to get a free, one-time limited month’s supply by going to NovoCare.com or calling 844-668-6463.
Sanofi’s Patient Connection program (888-847-4877)
In addition to drug company programs, Sagall suggests consumers look into diabetes clinics and diabetes-specific organizations within their state or counties. Those may also offer low or no-cost insulin. To find one near you, contact a customer service specialist at Needymeds.com or 800-503-6897 for free help.
Consider an Older Version of Insulin
Insulin is a naturally occurring hormone, and for decades, insulin used by humans was derived from pigs or cattle. Today, insulin is cultivated in a lab, with the most common type called human analog. It's designed to be more quickly and consistently metabolized by the body, and consequently, it's more expensive.
But an older type of insulin, simply called "human insulin," is still sold today, and may work for some people, says Novo Nordisk's Inchausti. He says half a million people rely on the company’s Novo Nordisk Human Insulin, which is available for about $25 per vial at Walmart or CVS pharmacies. Eli Lilly’s, called Humalin, cost $148 per vial. Your insurance may cover some or all of that cost.